The question that we wanted to cover is a basic principle of ICD-10 coding. The question is first listed or principal diagnosis: how do we determine which to use? It’s important to know that the terms are somewhat interchangeable for inpatient and outpatient. But you have to understand what they mean and their purpose; otherwise, if you say the wrong thing for inpatient or outpatient, somebody might balk at it and say, “Oh, that’s really a principal diagnosis, not a first-listed diagnosis.” But honestly, what you’re doing is you’re determining which code gets sequenced first and billed out first.
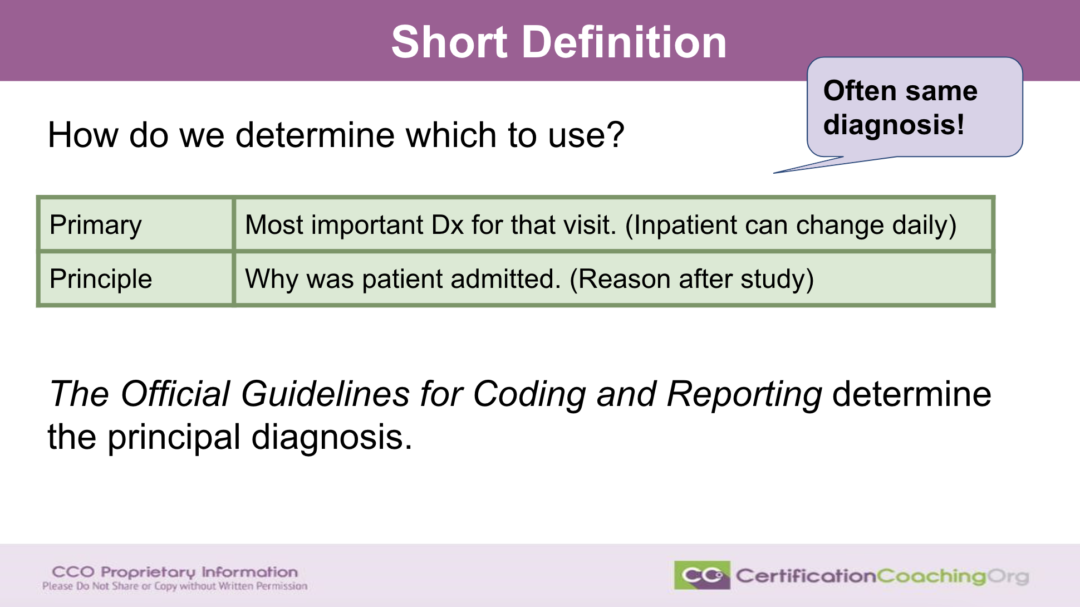
If we look at our short definition, we first need to see what’s the purpose or the use. I took the long definition and just tried to shorten it and comprise it, as to what does it actually mean? When you look at primary versus principal diagnosis, the primary diagnosis is the most important diagnosis of the visit. When you look at inpatient, then that could change daily. Day 2 that the provider goes in and does his rounds and they’re doing progress notes, what is the most important diagnosis that day that they’re dealing with. The next day may be a completely different diagnosis.
What you’re going to do in inpatient is review those every single day and you are also considering things like DRGs. We’re not going to talk about those. There are resources and we talked about those more in-depth at another time.
Principal diagnosis is going to be why the patient was admitted, or why they did the study or testing, diagnostic or even any type of evaluations, things, why was the patient admitted, the cause of that. You may not know that right away either. They may have multiple diagnoses. Most of the time though, the principal and primary and inpatient are the same diagnosis, but it doesn’t have to be that way.
It is also noteworthy that it really doesn’t matter what the sequencing is that the provider puts in as far as diagnosis A, B, C or D. It is really all up to the official guidelines and the coding clinic that we’ve been getting to give us direction whenever there are some black and white areas that we can’t call black and white, that become gray or muddied, that’s their purpose of the coding clinic.
One of the key components of your certification or if you’re getting ready to test for your certification is understanding those official guidelines both for all of the code sets that you’re dealing with. Principal and primary diagnosis a lot of times, especially inpatient can be the same diagnosis when we look at outpatient, what was the reason the patient was seen for that day? Can there be multiple conditions that the patient was seen for that day? Yes, just like inpatients. So, then, we look at what is the diagnosis that caused the most medical decision making, that would be the number one diagnosis. If there’s multiple that are equal when you go to look at them.
Z Codes
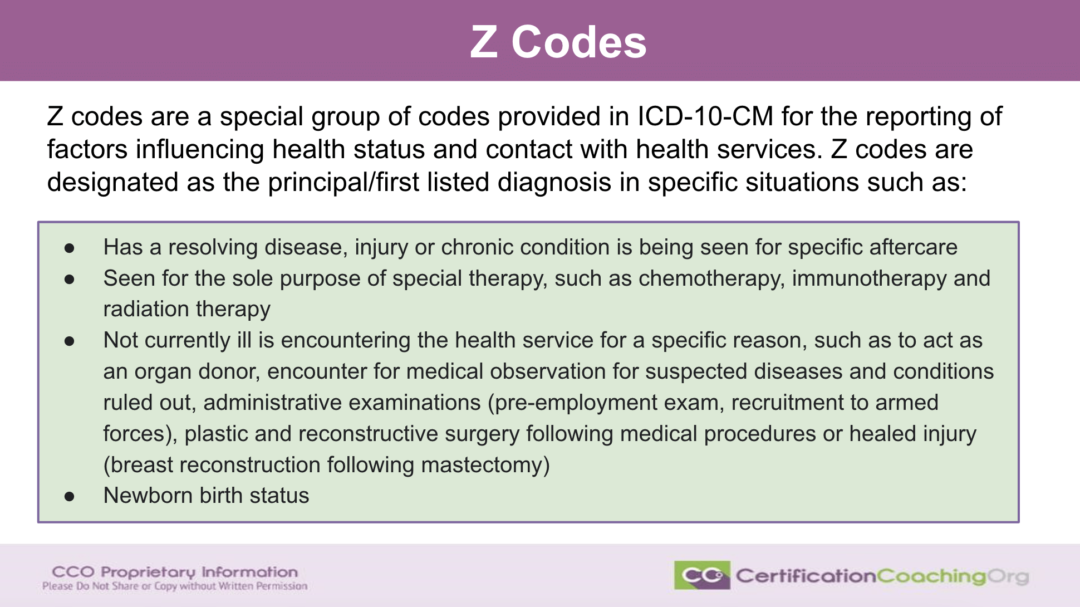
Can Z codes be used as first listed or principal diagnosis? Absolutely they can be. Not all of them but let’s look at the different ones that could be. I didn’t pull out the codes and give you code ranges, I just broke down the purpose of the Z code. If we have a diagnosis and there is a condition that’s getting results, then it might be an injury, chronic condition, after care, those all can be used as the purpose for the patient to be there that day.
What if it’s for therapy – immunotherapy, chemotherapy? Don’t just think like physical therapy. Often the patient needs to be seen not because they’re sick but because of another specific reason and those are broken down, there are pre-employment exams, recruitments to the armed forces, we don’t think of those. What about school physicals? Administrative exams like pre-employment exams? Did I already mention that?
Also, they mentioned plastic and reconstructive surgeries, say a patient goes in and has bilateral mastectomies and they’re doing the reconstruction of the breast, so in other words there’s really not anything wrong, but they have to follow the care.
Don’t forget the status of newborn babies, we use a Z code for that. There’s nothing wrong with the baby but we do have to cover the status code.
Multiple Diagnoses
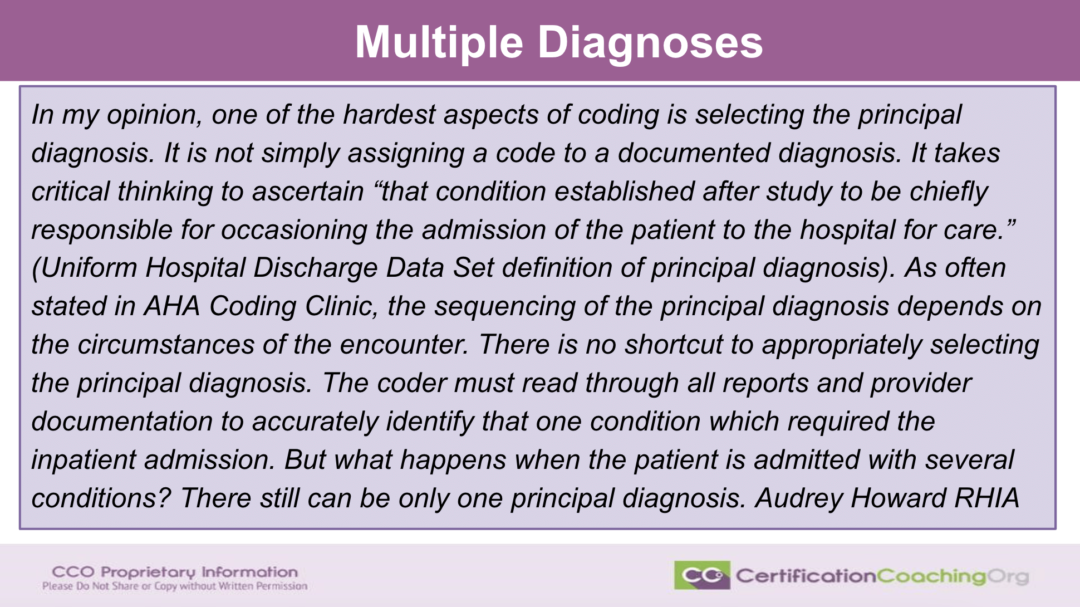
I found a great article that was by Audrey Howard, she’s an RHIA with AHIMA and she mentioned multiple diagnoses, how she determines the principal diagnosis when there’s multiple diagnoses that carry equal weight. I really, really like the statement that she made so much so that I put the statement here for us to look at and then I wanted to take us out to where the article was written for 3M. I wanted to show you some of the examples that she gave here. I could easily have just give her attribution and put it on the slide deck, but again this is just a little tip of how you can do some research and how you would navigate an article per se and get examples and hopefully that would assist you in understanding.
What Audrey says is that in her opinion one of the hardest things she does when dealing with coding for inpatient is to get that principal diagnosis and she goes on to state that it’s not simply assigning the code to whatever the documented diagnosis is, there could be multiple diagnoses. She states it takes critical thinking to ascertain “that condition established after study to be chiefly responsible for occasioning the admission of the patient to the hospital for care.” This is a direct definition from the Uniform Hospital Discharge Data Set and that is abbreviated UHDDS, you may be familiar with that if you’re dealing with inpatient coding, then you probably are.
She also goes on to talk about the AHA Coding Clinic that many of you probably use often and they have education or what they’ve determined as guidelines when you get into those gray areas. If you don’t already have a coding clinic, your employer may offer a coding clinic for you. If you are working as a coder and you don’t know if you have access to a coding clinic, you might go ahead and ask if maybe available and you didn’t even realize it.
There is really not a shortcut. You’re going to have to put in the homework and look at all of the information to determine, especially from day-to-day, that it can change, is what’s the diagnosis for that day. You got to go through all the reports, you got to go to the provider documentation; a lot of times there’s multiple providers that you’re dealing with in the inpatient word, and you have to look at several conditions happening at once, most of the time, to come up with one diagnosis out of all of the diagnosis.
Let me pull that article over at 3M. I want to make sure that you’re able to see it well enough. I’m going to see if I need to make this a little bit bigger. The link I put in the resource slide at the end of the slide deck so that you can have access to that and I hope it’s beneficial to you.
She wrote this back in June 2020, but it’s still applicable for today. This is where I got her discussing that. Then she gives examples of how she determines what is going to be that diagnosis. She says: “I ask myself these questions” and that’s another reason why she resonated with me when I read this article because I’m always telling myself. You have to ask yourself this question and then that will give you the answer, you’ll be able to break it down and determine.
First thing is: Did the condition necessitate inpatient admission? Would the patient have been admitted to the inpatient setting for this condition? Was it diabetes? Was it the COPD exacerbation, was it the pneumonia with an exacerbation, etc. Then, it goes to say: Did this condition meet the admission criteria? Was the patient sick enough? Was the treatment significant enough?
In other words, the patient may have diabetes, but the reason that they were admitted, what was complicating the problem, the reason the patient just couldn’t go home was the exacerbation of their COPD. Then, could this condition stand alone for the reason of the admission?
Go through this checklist. Ask yourself when you’re doing inpatient coding those questions. She gives an example and let’s look at this one. Then, we’re going to look at this briefly because you can go out and spend more time. But give an example of a 65-year-old female, she goes to the ER and she has a chief complaint which is signs and symptoms of weakness, fatigue, shortness of breath on exertion for the past week. She also complained of dysuria for the past month. The patient is alert, cooperative, and in no apparent distress without fever or chills. Her chest was clear bilaterally with no rales, rhonchi or wheezing. No accessory muscle use or stridor.
In other words, they’re ruling out everything for a lung condition.
Then, her COVID-19 test came back negative. She has no known exposure and she was noted to have 3+ bilateral pitting edema up to the knees.
That takes you in a different avenue. The lungs are kind of OK, something’s happened with the heart.
The following table shows a summary of the pertinent information.
What did they do? They said she had the signs and symptoms of upper respiratory infection, possibly it could be sepsis, and so they list off signs and symptoms, all the lab tests and the treatment, they put her on IV antibiotics right away.
Condition: deep venous thrombosis, because she had the bilateral pitting edema. They did ultrasound, etc, all those tests. They did heparin and Eliquis. Then, pulmonary embolism, not documented by the provider, though, and that could explain the shortness of breath and then they go on and review the lab test, the heparin that they use and Eliquis.
She puts in there that the final diagnoses included the UTI and DVT. Sepsis was ruled out. When you break that all down, what did she go with based on the circumstances? The only option for the principal diagnosis was the UTI: a query related to pulmonary embolism would have been appropriate because the DVT was not supported as a principal diagnosis. And then again all that you read the rest of that, but she also gives examples of worsening kidney function, going from one facility to another.
I really, really enjoyed the article. I thought she explained it very well and I encourage you to take advantage of searching articles such as that, when they come from a reputable source. 3M would be a reputable source. Her credential tells you she’s a reputable source and she has experience in this realm.
Outpatient Coding Diagnosis
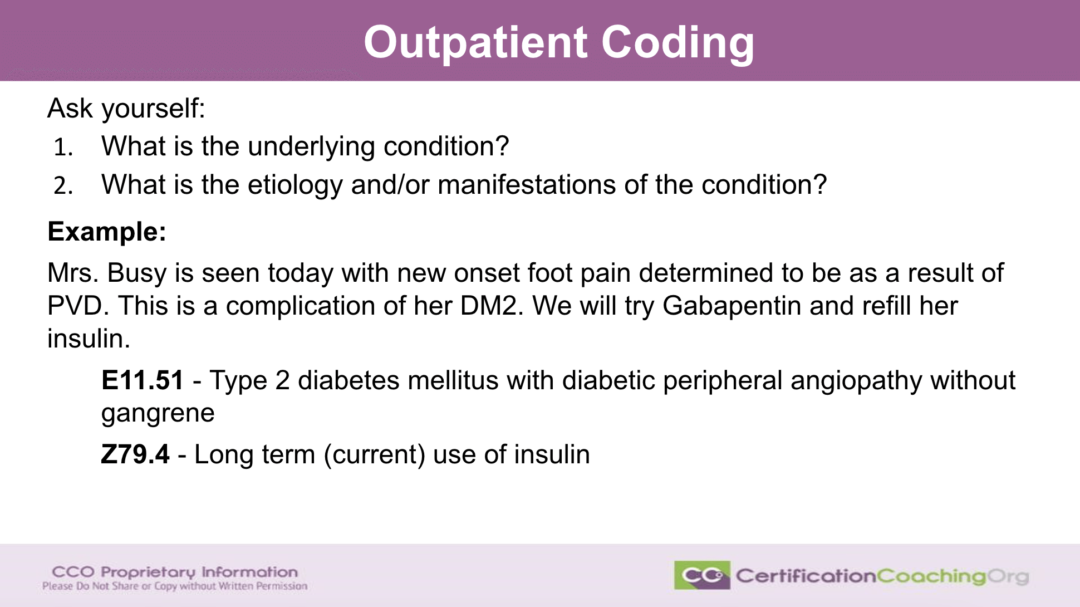
What about outpatient coding? This is the way I like to do it just the way she did. Ask yourself: What is the underlying condition that the patient has and what’s the etiology and/or manifestations of the condition? I gave you an example. We got Mrs. Busy (I made this really simple), she’s seen today with new onset foot pain determined to be as a result of PVD. This is a complication of her diabetes (thank you provider for mentioning that and telling us what type of diabetes she has), so they are going to put her on gabapentin and they’re going to refill her insulin. That tells us that we would have had three diagnoses if PVD had that relationship with diabetes, so we get to use a combo code, so we’re able to code the E11.51 – type 2 diabetes with diabetic peripheral angiopathy, which is PVD. They don’t have gangrene and also she’s on insulin.
We wouldn’t use the Z79.4 as the first diagnosis because even though he refilled her insulin and that may have been one of the reasons that she was there to get more refills on her insulin, still what caused the most consideration and concern in medical decision making, it was the fact that she had a new sign and symptom and he gave her a new diagnosis, PVD. It also was complicating her diabetes, so we’ve got multiple, two diagnoses going there. E11.51 would be that first-listed diagnosis.
I’m seeing a question here: “Good evening, I’m having some trouble with diagnosing 4 to 5 for one patient. I’m having issues with that portion of my classes.” I can give you a quick little tip, Matilda. Again, why was the patient seen that day? That’s usually the first-listed diagnosis. However, if there is a diagnosis that is more severe, you would use that first, however, you still have to follow the guidelines and if you’re in a course that’s what they’re driving home. Also, this pertains to CPT; there’s sequencing of CPT codes. A lot of students get confused with repairs sometime on removals of lesions and things will get sequenced before the actual removal because it’s more complex than just cutting off that lesion. They have to do a repair that takes more time and underpinning and stuff like that. Again, follow what the guidelines state, if the guidelines use the term code first, then you know that code is sequenced first. If they use the term “use in addition” that code is sequenced second. We have lots of practice, so feel free to jump in and look at a lot of our YouTube videos regarding that.
“My past, if a patient had 3 or 4 diagnoses, list them all each day. Inpatient status follows the ICD-10 rules related to add a diagnosis or excludes, rules 1, encoder stuff will inform you.” That is correct, Jane. It’s not like you’re thrown out there to do all of this guesswork, you have the tools especially in inpatient to be able to determine which is the proper code to work with.
“What is the doorknob diagnosis, I’ve heard that expression.” I’m not sure about doorknob diagnosis, I think that refers to when the provider first opens up the door in the patient’s room, doorknob, what they’re thinking they’re going to see.
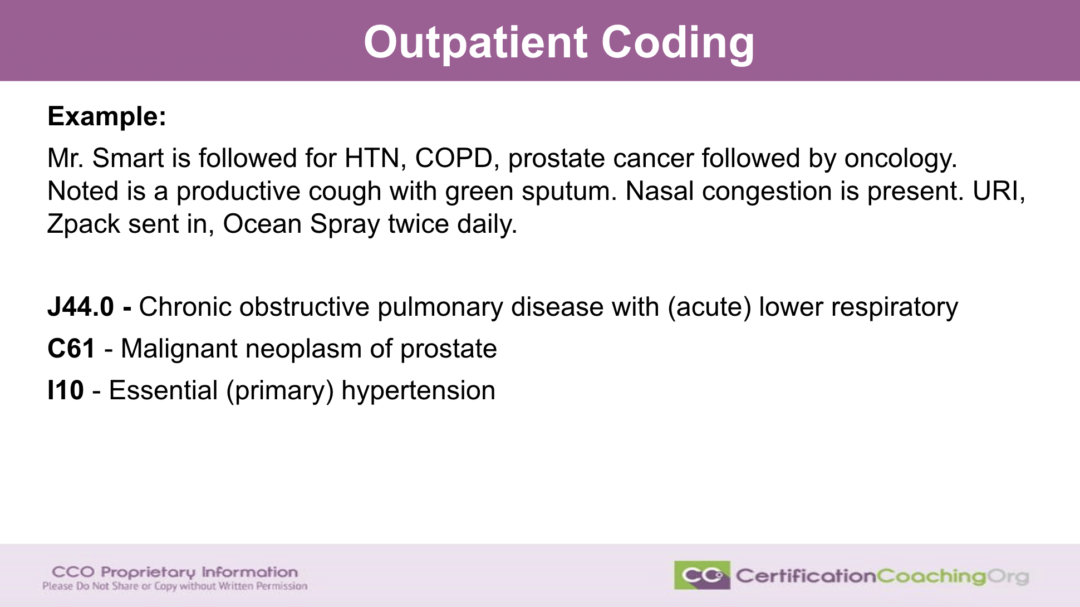
Let’s now look at another example that real quickly we have Mr. Smart and he’s going to the doctor. He’s PCP and he’s being followed for his hypertension, his COPD, his prostate cancer which is followed by oncology. Today, he states “noted is a productive cough with green sputum. Nasal congestion is present. URI is the diagnosis. Zpack is the plan of care,” that’s sent in to the pharmacy and he tells him to get an over-the-counter Ocean Spray and to use that twice a day.
We have three diagnoses, we have COPD, we have hypertension and we have prostate cancer. Now, you would assume if you’re talking about severity of disease processes, prostate cancer would trump everything else because that’s a more severe active prostate cancer, that should always be number one. However, that’s being managed by oncology and even though that’s part of the medical decision making that the provider is doing that day, we have to think, “OK, we’re in active treatment for prostate cancer,” or whatever the treatment is, we have a patient that actively has cancer and they also have hypertension and a lot of medications that you give a patient even over the counter can affect hypertension medication.
But what is the reason? We don’t even know the reason the patient came in, per se, he’s being followed with these three diagnoses. But the patient does have a productive cough. The sputum is green; they’re probably sending it off to have it checked to see what the organism is. In the meantime, the patient also obviously has some type of a cold or something going on, so they give them a respiratory infection diagnosis.
We have the J44.0 because it’s not regular COPD; we have an exacerbation going on. Also, don’t worry about it being lower respiratory infection versus upper respiratory infection. Then, next the most severe out of the other two would be the fact the patient has cancer, C61, and oh by the way they do have hypertension. So that is the sequencing of today’s visit.
If they were having complications due to the prostate cancer or any of the treatments for the prostate cancer, say nausea, vomiting as a result or dehydration due to the chemotherapy, etc, that changes the sequencing. But again, just keeping it short and sweet with the information that you’re provided, it would be the COPD first, the neoplasm after that, the prostate cancer and then anything else that followed in the sequence from there.
Don’t forget that more information could be found in the CCO Club. If you’re watching us on YouTube, don’t forget to subscribe so that you can see our other videos and know when we are about to have a live video. We do all of these live; some we keep on YouTube and some we put exclusively into the Club. Don’t forget that we have fabulous courses if you want more information, but if there is a question that you have and that you want us to unpack and talk about it, go to the Topic Request area and we will absolutely put it in this format and hopefully answer your questions.
![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)
