
Video Transcript (Starting at 24:40)
And now for that big debate I was telling you about. I guess since I’m on the left, I should give my point of view first. Chandra could follow –
Coach Chandra: You go first.
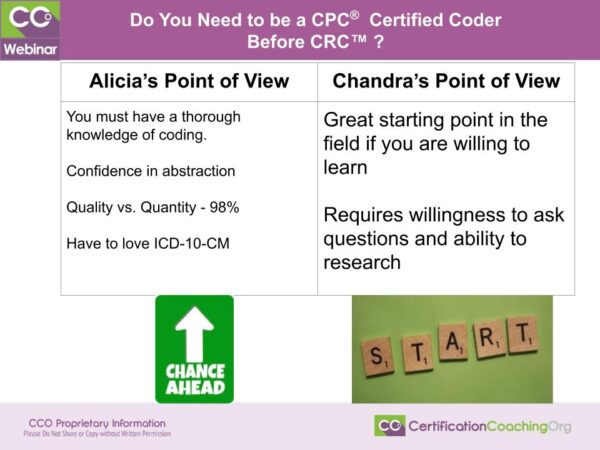
Coach Alicia: Okay. She could follow up. I never was in debate class. However, we both have very valid points. I like to think of it like this. We come at risk adjustment from two different angles. Like Chandra said, her role had been working mostly for – not mostly but predominantly a lot of the work that she had been doing is the auditing aspect. She’s going in and looking and educating about risk adjustment, that behind the scenes, why we do what we do. And so that’s another viewpoint.
Where my viewpoint is, from what I like to call, “in the trenches” coding. So I work for an MA plan and so therefore I was doing, well, it’s not grunt work but I like to think that Chandra was up here in the office and I was down here in the trenches. There’s so many aspects of risk adjustment. So my point of view is that if you’re going to do risk adjustment coding and you’re doing charts all day long, you really have to have a firm foundation in coding. Not just ICD-10. Now you need to really know ICD-10 and you need to enjoy diagnosis coding. I have to say, well, you have to love it. But when you’re taking a course, another thing that it does is it allows you experience in both CPT and ICD. I’ve had enough students through the years to say, you know, I’ve got some that say “I absolutely love working with diagnoses” and then you have another group that says “I love CPT.” So if you really love CPT and E/M work and stuff like that, well then risk adjustment may not be a good fit for you. And you would learn that by taking a course.
It’s a lot of abstract work, abstracting the diagnosis, but not just the diagnosis. You need to be able to abstract a line. If the document states that the patient has diabetes but you cannot prove in that encounter that the patient is actively being treated for diabetes and then, you know, pull out other little nuances and information about the condition then, you know. You’ve got to be confident with your abstraction.
The other thing is with risk adjustment, it’s quality versus quantity. People used to say, way back in the day, why do inpatient coders get paid more? Well, it involves a lot more money. Right? If you’re working for a physician, you’re dealing with a certain amount of money that’s coming and going, that you’re not really in charge of but you understand that your coding makes a difference versus inpatient, you know, and there’s more documentation and so on and so forth. That’s the same way it is with risk adjustment. We’re talking about a lot of money and they don’t want you to make a mistake.
So it’s kind of on average they tell you, you know, with coding, I like to say standard coding meaning all the other coding not risk adjustment, it’s about a 95% accuracy rate when you’re audited and everything. With risk adjustment, it’s 98% or 99% accuracy rate, and you’re constantly audited. Now, that’s not an oppressive thing. It’s a good thing because you’re constantly learning. And so a person that’s been coding or had a course and got their CPC, I feel like they’ve kind of been through all of this. They know what they’re getting into and so therefore they can go in with an open mind and they’re more flexible. Their knowledge base is just bigger.
And now I’ll turn it over to Chandra and that she can attempt to explain why you don’t need a CPC.
Boyd: Thank you for being so gracious to not hog the floor, yeah. Thank you.
Coach Chandra: Well, the first thing I want do is based on some of the chat questions, let’s clear up a little bit here. Risk adjustment coders do nothing with CPT codes. Would you agree?
Coach Alicia: Yes. They don’t touch them.
Coach Chandra: And the CPT codes are nowhere on the CRC exam. Neither are ICD-10-PCS codes. There are no procedure codes used when we’re doing risk adjustment coding. Risk adjustment is based on diagnosis codes and it involves, just as Alicia said, a very thorough understanding of the disease process – anatomy, pathophysiology and how a disease evolves over time especially if left untreated, what treatment measures are available, those types of things.
But my perspective on this is that I think risk adjustment is actually a really good starting point for many, many individuals in the industry. Some people will say, well, certain employers won’t hire you for risk adjustment unless you have a CPC or a CCA or either an AAPC or an AHIMA credential. I would say okay, I understand that. The risk adjustment credential, the CRC has only been around a little over a year. So it hasn’t gained as much traction as some of the other credentials that have been there a lot longer. However, the more employers in the risk adjustment arena that learn about this credential and figure out how the testing is done and that, well, okay they don’t really… you know, if you get someone who has a CPC, there’s no guarantee that they really are comfortable with diagnosis coding. They have to be able to diagnosis code, I’m not going to argue with that at all. And they have to have a baseline understanding of anatomy, med terms, that sort of thing. But there’s no guarantee that they’re really strong in diagnosis coding and disease process. The risk adjustment credential tests you more heavily from a coding perspective on diagnosis coding and disease process.
So it’s why I say from my perspective, this is a great jumping off point for some people because I’ve had a number of people come through my courses over the year, not just here at CCO but when I taught at colleges in the past and different arenas, what you find is people either love CPT or they love ICD, one of the two. And I had a greater majority of those that once they really understood diagnosis coding and that condition was not a word you could look up in the index, that they understood it and they’re like “okay, this is easier.” Well, it’s easier in my opinion to begin to teach those individuals the disease process, how it evolves and how diagnosis codes are related. But it requires a lot of the person getting into the field. They’ve got to be willing to ask questions. They’ve got to be receptive to constructive criticism. They’ve got to understand, just as Alicia said, that auditing aspect. You’ve got to be at a very, very, very high level of accuracy consistently.
And I would agree that it is a quality over quantity, but that’s for a set amount of time. The quality always stays there but they do begin to push a quota the longer that you’ve been with any organization. And it’s kind of one of those for those that recognize it, I’m seeing a lot just via social media and all of the different job boards that we follow and all of that, there are more and more employers that are willing to hire certified individuals that have either a CPC or a CRC with little and sometimes even no experience to do risk adjustment because there aren’t any bad habits they have to break. They think, I can teach these people how to code exactly what I need them to code and how to interpret this documentation. And I will tell you, most employers you go through have a pretty rigorous training process and it’s, just as Alicia said, you’ve kind of got a bible if you will that you live by in addition to your code book to help you clarify when you can code certain things and when you can’t, and you’re constantly audited and given feedback. And your audit results determine what you get in your cue the next day. That sort of thing. So that’s kind of my perspective.
Coach Alicia: And I add that, in my opinion, if you’re not certified and you’re a clinician, the CRC is a great jump, you know.
Coach Chandra: Absolutely.
Coach Alicia: Because you’re already licensed. So that’s a really good step. Or even a transcriptionist, great transition. Yeah. So there you have it, both of our opinions.
Coach Chandra: Yeah. The more clinical knowledge you have, it’s actually a benefit with the CRC. The only problem that I see typically with clinicians – and Alicia, I think you’ve probably seen this too – they have a very hard time shutting off their clinical mindset actually writing down certain codes. Right? They see this process and they know where it’s going. Just because you know it’s going there doesn’t mean you can code that final code.
Coach Alicia: Right.
Coach Chandra: If the doctor didn’t call it that. You’ve got to have all of the linking statements and the right information written in the chart, and that’s where I see many, many clinicians especially a lot of the nurses that I’ve worked with. They’re like, “That’s just so hard.” I know. “I can see where the patient’s going,” and I’m like, I get that but you only code what’s in the record.
Coach Alicia: They overthink. And it’s really hard to rein yourself back in when you have vast knowledge on something and so some of them really struggle with that. But once they realize you do it, then it makes it easier. But they tend to do that.
![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)