Chandra: CRC Certification — For those of you who have been waiting for this course, we thank you so much for hanging in there with us. We wanted to make sure that this is the best course that we could possibly give you. And I love the statement at the top of this slide that says: A Complete “No-Fluff” Course. What we’ve done is we’ve taken our existing Risk Adjustment course, we’ve streamlined it, and we have bulked it out, we have added all sorts of just amazing content. I’m fascinated by the stuff that our subject matter experts have provided and the amount of content we’ve been able to add.
VIDEO: Why CRC Certification — Certified Risk Adjustment Course 2.0

When we look at the things that we offer for Risk Adjustment, we have our full course, we also have a Risk Adjustment Blitz, that is that Risk Adjustment Blitz, does not go through the coding components. It assumes you already know how to code. It goes through all of the other things that the AAPC tests you on in the CRC, all of the regulations, all of the different legislative pieces, all of that sort of thing.
Then, we also have the ICD-10 Review Blitz. These are all bundled together when you purchase our Risk Adjustment Course, so when you purchase the Risk Adjustment Course, you get the CRC Review Blitz and the ICD-10 Blitz, so that you get both pieces, the coding and everything else.
Why would you want to think about this Risk Adjustment?
First of all, we’re still in the early bird pricing for our Risk Adjustment Course Version 2.0. I will say when you buy Version 2.0 right now, you’ll get access to 1.0. When 2.0 goes live at the end of the month – it’s June 30th is when all the content is going up – you will have access to Version 2.0 as well. So, you get both, you get Version 1 and Version 2; so you’ll get all those different recordings and all the different contents that’s there.
Boyd, can you remind me, early bird pricing, it’s $100 discount, right?
Boyd: Yeah. That’s the last slide here. This slide was really just to point out for people, it’s like, what is the CRC in a nutshell and why would they want to be thinking about it, and then this slide goes into that contents and courses.
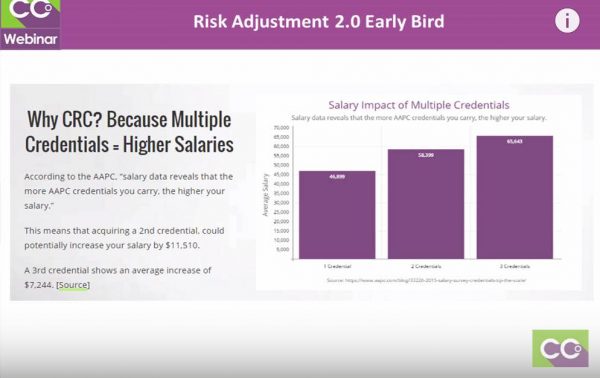 Chandra: OK. The CRC Certification / Risk Adjustment credential oftentimes winds up being an additional credential for most people. They already have their CPC, but they really like diagnosis coding, there’s a high demand for Risk Adjustment coding. I’m going to talk about that for a minute. Having more than one credential always opens doors for you. There are just more areas that you can get a job in than you could with just one credential. Employers tend to recognize that.
Chandra: OK. The CRC Certification / Risk Adjustment credential oftentimes winds up being an additional credential for most people. They already have their CPC, but they really like diagnosis coding, there’s a high demand for Risk Adjustment coding. I’m going to talk about that for a minute. Having more than one credential always opens doors for you. There are just more areas that you can get a job in than you could with just one credential. Employers tend to recognize that.
You’ll notice based on the AAPC salary survey, you do see an increase in average salary payments, in opportunities based on the number of credentials that you have. I’ve had a number of people and I want to make sure I point out, there’s been a lot of talk on social media about risk adjustment and HCC coding being an unstable field. That’s not necessarily true. In the past, yes, many employers hire kind of seasonally. They shouldn’t have been, they’re required to report codes all year long, but oftentimes they waited till the end and now it’s clutch time and they hire all these people stop, they do it all over again next year.
What we’ve actually seen in the last, I would say, probably 12 to 24 months, is more employers staffing that out, getting consistent staff, building good staff, to be collecting this information year round. That’s because in the past it’s been mainly risk adjustment plans for Medicare, and now we have risk adjustment plans for not only Medicare, but Medicaid as well as the Obamacare Plans. So it has taken on a huge piece of the marketplace. You just need to research the employers that you’re applying with, quite frankly, and know what their process is and what their stability is, that sort of thing.
But there are a lots of really good risk adjustment employers out there who are looking for coders, looking for coders who do not necessarily have a lot of experience. They’re more concerned about you having their credential and they want to teach you how to do it their way, so we’re seeing more and more hiring those that may not have a lot of experience, if any experience, and many of the risk adjustment positions are remote positions. Anything I’m missing there, Alicia?
Alicia: Yeah. I want to say that things have changed, or I would tell people from five years ago or even three years ago compared to what it is now, I think risk adjustment has made that happen in some ways, but these companies are hiring CPC-As, so never fear the “A” if you’re a new coder. But what they want with risk adjustment is quality over quantity. You may hear them say you need a 95% accuracy rate when you’re audited.
One thing, know that with risk adjustment, you better not be able to… I’ll say a chip on your shoulder or something, you will constantly be audited. You will even eventually be asked to audit other people, but auditing is a way of life with risk adjustment so you have to be good with that.
Chandra: You’ve got to be receptive to feedback, you’ve got to be willing to… I won’t say argue, but…
Alicia: Positive attitude.
Chandra: You’ve got to make your case and you got to make your case without making other people mad. Give the facts and explain, “Here’s where I was coming from, can you…” You got to be able to do your research, that’s huge.
Alicia: Since Chandra has also said that this is predominantly now a remote-type position. There are other places, facilities, that are hiring groups and things, but it’s mostly remote. One of the things I think that has been impacted by that is that as of 2014, everybody had to go EHRs; now we don’t have to worry about all the handwritten stuff like we used to, so it’s kind of conducive. Society, we’re changing, but…
Chandra: Let me jump in there. Even those physicians who are not on electronic medical record, many of these risk adjustment positions are not working for the physician, they’re working for the payer, they’re working for the insurance carrier. If you don’t know what I’m talking about, that’s a topic for a different conversation because it’s understanding how risk adjustment really works.
The easiest way to say it is the carriers are paid by the Federal government based on the claims data they get from the physicians, so think of the carrier as the middle man. They’re taking all the data that they got from the physician and they’re refining it, picking the best ones and sending it up to CMS or whatever federal entity is paying them to justify those claims. That’s where many of the risk adjustment coders’ work are doing that validation for the payer. So, they have the records, are already there and they have scanned them in even if they are paper records.
Alicia: Right. I want to also throw in there, the CRC certification is a new credential, so is it even a year old yet? I don’t think it’s a year, maybe. So, that being said, new credentials take time to hit the traction in the arena, so they’re not requiring now that people have the CRC certification. If you go ahead and have your CRC and you’re credentialed, and then you walk in for a position, that’s going to change a lot for you. That’s going to open doors and you will end up being in a more of a supervisory or even an auditing… your role will change. However, if you walk in and say, “I’m a CRC,” they may not even realize what that is. So, when it does hit, I foresee that they will start wanting you, require you to have that eventually.
Let me go to the next slide. Chandra, you can go over the components of the 2.0.
Risk Adjustment 2.0 Course Contents:
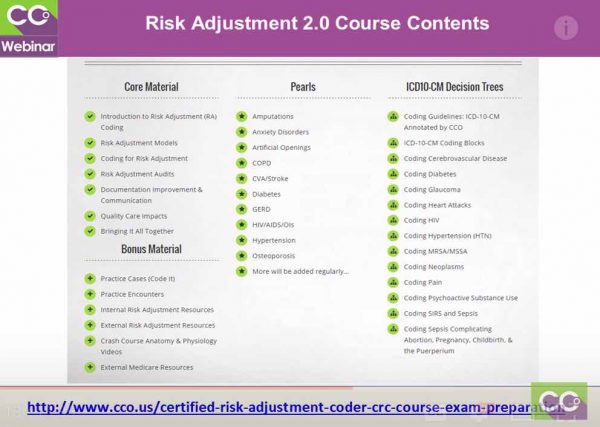 Chandra: This gives you a breakdown of what information is included in the 2.0 course. This is actually not a comprehensive list. It is for the course material. What we’ve done is in version 1, I believe we had 16 chapters, they were small and the flow, [we had feedback that “it could flow a little bit better for us”].
Chandra: This gives you a breakdown of what information is included in the 2.0 course. This is actually not a comprehensive list. It is for the course material. What we’ve done is in version 1, I believe we had 16 chapters, they were small and the flow, [we had feedback that “it could flow a little bit better for us”].
So, we sat down, we looked at it, we said, “OK. We’re going to streamline everything. We’re going to take it down to seven modules; we’re going to combine the things that are similar together.” Like, for example, the quality care impacts, that include STAR and HEDIS and a little bit about meaningful use; rather than have them in three separate chapters. Kind of pull them all together and just move everything so that it’s a little easier to follow through.
There’s a lot of bonus material, we’ve got practice cases, practice encounters, internal and external resources that we found or that we’ve developed, all sorts of cheat sheets for how to better analyze certain diagnosis. These Pearls, and Alicia is actually going to go through one of these for you guys tonight on this call, but the Pearls are going to be huge in value. Pearls doesn’t stand for anything, we just talk about being like a coding gem. It’s something that’s indispensable. These Pearls will go through the definition of a disease, what the guidelines are that are applicable to that, how does it break down in ICD, what coding clinic information do you need, the anatomy and medications and all of that stuff. So, you have one central resource per disease. When the course launches though, it will be about 20 of these in there, and we’ll continue to add to them as time goes on.
Then, we have some Decision Trees that we’ve created based on the ICD-10 guidelines to help you navigate through how to select the right code and to really learn the guidelines for ICD-10. If you’re not familiar with risk adjustment coding, the one thing I want to point out, there is no CPT and HCPCS involved in risk adjustment coding. You live and die by your ICD-10-CM manual. There is no PCS coding, no CPT, no HCPCS, it’s all ICD-10-CM all the time. The more comfortable you are with disease process, the better adjustment coder. Wouldn’t you agree, Alicia?
Alicia: Oh, yeah. That’s what I like. Again, if you are taking a coding course right now; for example if you are taking PBC course for the CPC, doing that will allow you to decide, “Hey, I really like the diagnosing aspect of what I’m doing.” Or you may say, “I really like CPT. I understand, I like E/M.” That can help you decide, is risk adjustment for me, or is maybe auditing or specialty in a body system? Take the time to do that, but like Chandra said, this is all diagnosis coding and the disease process, which again I absolutely love. You got to continually increase your knowledge-base on the disease process because you do have to know the treatments that are applicable, you just don’t have to code them.
Boyd: Chandra has recorded a nice video for you as well, and it goes more in-depth. There’s also a frequently asked questions section there, so you can click on those plus signs and those are the most frequently asked questions about the course.
Alicia: Just to see if it works for you. Chandra did all the recordings, the existing version I did them, and Chandra these, so would get access to both of them. But, really truly having them all streamlined is going to make it much easier to get through them. We have a lot of people that did very well with the course and passed their CRC, but again, like I mentioned earlier in the webinar, it’s one of those mind blowing “pahhh”! It’s going to be exciting.
Related CRC Certification — Risk Adjustment Course Posts:
- ICD 10 Impact on Risk Adjustment | Risk Adjustment Training Video
- Introduction to Risk Adjustment — HCC Coding – Video
- CCO Risk Adjustment Course Version 2.0 – Video

![[CCO] Certification Coaching Organization LLC [CCO] Certification Coaching Organization LLC](https://www.cco.us/wp-content/uploads/2015/05/CCO-Logo-2015-d3-500px.png)